
Data Integration
We've developed a unique set of processes to combine and analyze clinical and claims data from our independent health systems into a single source. This allows employers to view their population holistically and identify trends earlier.
The foundational element of our program is clinical and claims data integration.
Integration of data across independent health systems
When a member renders services from their primary care provider in one health system and visits an urgent care clinic in another system within our clinically integrated network, Embright integrates the records for the member.
Embright connects and integrates a member's data across our health systems, and the providers delivering care have a more complete view of the member's care and claims history. This integration benefits the member, provider, and employer.
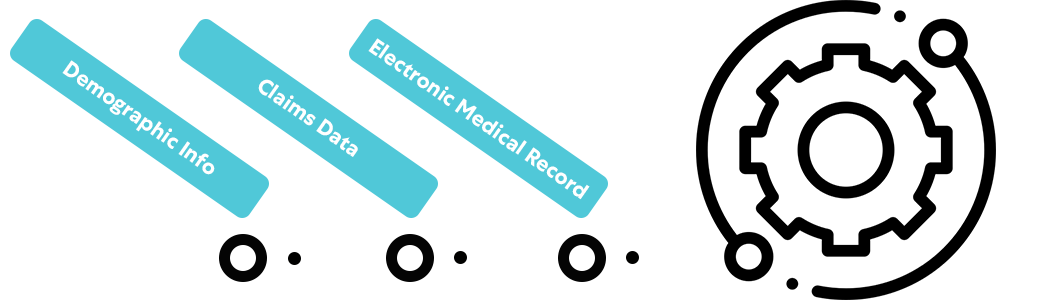
Unified member profile
We collect a member's demographic information, historical claims, and electronic medical record (EMR) to create a 360° view across health systems.
Healthcare, health plan, and population health benefits
Embright's unique data integration process benefits the individual member, the employee population, and the employer sponsoring the health plan. By collecting and combining the data across our award-winning health systems, employers have a more holistic view of the healthcare services rendered, utilization patterns, and cost allocation.
Holistic View
Employers gain access to a more complete view of their population from the combination of clinical data across independent health systems and historical claims in a single source.
Understand Trends
Easy-to-use and regular reports are available to employers outlining population utilization patterns, population health trends, cost allocations, to name a few. Report guidelines align with the shared goals set between the employer and providers delivering care.
Implement Adjustments
With direct access to providers, employers can make health plan adjustments mid-year or annually to encourage change in member behavior and curb spending.
Integration and the member experience
Members benefit from our data model and clinically integrated network through enhanced care navigation, access, and coordination.